Characteristics, causes, symptoms, transmission routes, and prevention of diphtheria
- Characteristics, causes, symptoms, transmission routes and ways to prevent diphtheria.
Diphtheria is an acute bacterial infection with pseudomembranes in the tonsil glands, pharynx, larynx, and nose. The disease can appear in the skin, other mucous membranes such as the conjunctiva or genitals.
According to the Health and Life newspaper, diphtheria is both an infectious and toxic disease and the serious damage of the disease is mainly caused by exotoxins of diphtheria bacteria.
It is important to distinguish leukemia from other pharyngitis with pseudomembranous pus or tonsillitis with pus cavity.
Overview of diphtheria
Diphtheria often appears during cold months in temperate regions. The disease is seasonal, often widespread, and can develop into an epidemic, especially in children under 15 years old who have not been fully immunized. - Incubation period: From 2 to 5 days, possibly longer.
Transmission period: Usually not fixed. Patients eliminate bacteria from the onset, possibly right from the end of the incubation period. The infectious period lasts about 2 weeks or less, rarely more than 4 weeks.
Healthy people carrying diphtheria bacteria can last from a few days to 3 or 4 weeks, and in very rare cases it lasts up to 6 months. Rapidly effective antibiotic treatment will end transmission. There are rare cases of chronic bacterial carriage lasting more than 6 months.
Diphtheria is transmitted through the respiratory tract through contact with a sick person or a healthy person carrying diphtheria bacteria. The disease can also be transmitted by contact with objects contaminated with excretions of a person infected with diphtheria bacteria. Raw milk can also be a means of transmitting diphtheria.
Symptoms of diphtheria
Clinical case:
Sore throat, nose, larynx. Red throat, painful swallowing. Pale skin, fatigue, swollen lymph nodes under the jaw causing swelling in the neck area.
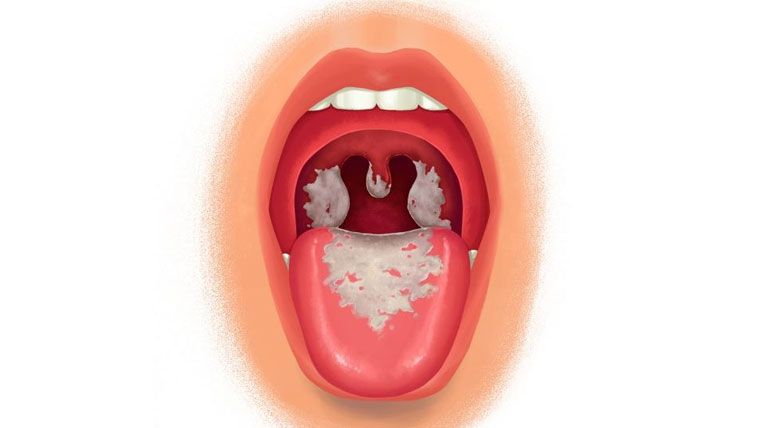
Examination revealed pseudomembranes. It is necessary to distinguish the properties of diphtheria pseudomembranes from purulent pseudomembranes. Diphtheria pseudomembranes are often ivory white or gray in color and stick tightly around the inflamed tissue. If peeled off, they will bleed. Put pseudomembranous membrane in a glass of water, even if you stir vigorously, it will not dissolve. As for pseudomembranous pus, it will completely dissolve in a glass of water. The mucosal area around the pseudomembranous membrane is hyperemic.
Laryngeal diphtheria is a serious disease in children. Clinical manifestations of local infection with diphtheria exotoxin are pseudomembranes and systemic manifestations are neurotoxicity, paralysis of cranial nerves, peripheral motor nerves and sensory nerves and/or inflammation. heart muscle. Mortality rate is about 5% - 10%.
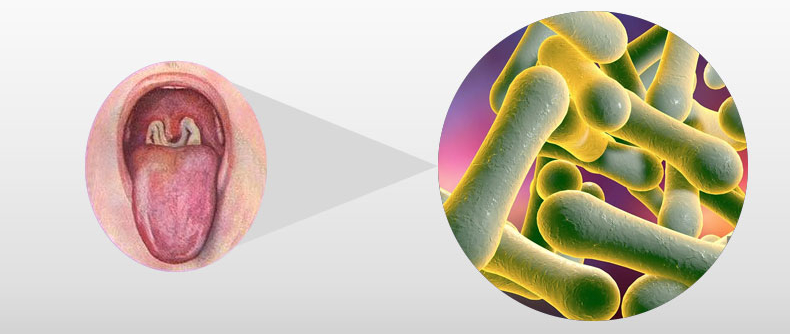
The causative agent of diphtheria
Diphtheria bacteria have 3 types: Gravis, Mitis and Intermedius. The shape of the bacteria is diverse, gram (+). Typically, the bacillus has one or two swollen heads, so it is also called a ball-shaped bacillus, 2-6 µm long, 0.5-1µm wide. Does not produce spores, does not move.
Bacteria have high resistance outside the body and can withstand cold and dryness. If protected by surrounding mucus, bacteria can live on objects for several days to several weeks; on fabric it can live for 30 days; in milk and drinking water, it can live up to 20 days; In a corpse, it lives for 2 weeks.
Diphtheria bacteria are sensitive to physical and chemical factors. Under direct sunlight, bacteria will die after a few hours, and diffused light will kill them after a few days. At a temperature of 580C, bacteria can live for 10 minutes, at 1% phenol and 60 degree alcohol they can live for 1 minute. Guinea pigs are highly susceptible to diphtheria bacteria.
The nature of diphtheria exotoxin is a protein with specific antigens, high toxicity, and cannot withstand temperature and formalin. The exotoxins of different types of diphtheria bacteria are the same.
Exotoxins, when treated with heat and formalin, will lose their virulence. This is called anatoxin and is used as a vaccine.
Transmission routes and symptoms of diphtheria
The World Health Organization says diphtheria is a serious infection caused by strains of bacteria called Corynebacteria diphtheriae, which produce toxins. Toxins often adhere to tissues in the respiratory system and cause illness by killing healthy tissues.
Typical symptoms of infection include sore throat, fever, neck swelling, and weakness.
Within 2–3 days of infection, dead tissue forms a thick, gray coating that can cover tissues in the nose, tonsils, and throat, making it difficult for the person to breathe and swallow.
More rarely, the toxin enters the bloodstream and causes damage to the heart, kidneys and nerves.
Diphtheria bacteria are spread from person to person, often through respiratory droplets, such as when coughing or sneezing. People can also get sick from touching an infected ulcer or open sore.
People at higher risk include household contacts, people exposed to patient secretions, and people who have frequent close contact with infected people.
According to BS. Phan Van Manh, Emergency Department, Central Tropical Diseases Hospital, the source of diphtheria is infected patients or healthy people who carry the bacteria but do not show signs of the disease.
The disease is mainly transmitted through the respiratory tract through contact with droplets from an infected person when coughing or sneezing.
In addition, the disease can be transmitted indirectly through contact with objects contaminated with nasopharyngeal fluid from a sick person or through contact with skin damaged by diphtheria.
Doctor. Phan Van Manh said that the most common form of diphtheria is in the respiratory tract (nose, throat, larynx, trachea), of which 70% is pharyngeal diphtheria. In addition, other locations can be infected such as cutaneous diphtheria, ocular diphtheria...
Cutaneous diphtheria can be transmitted sexually
In 2008, the authors of the Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India published in the Indian Journal of Dermatology, Venereology and Leprosy. Rare case of wound-borne diphtheria masquerading as a sexually transmitted disease (STD).
This is a 41-year-old man, married but sexually promiscuous, who came to the sexually transmitted disease (STD) clinic with multiple ulcers on the scrotum and genitals over the past 20 years. day.
Bacterial culture from specimens taken from genital ulcers grew morphologically and biochemically characteristic organisms of Corynaebacter diphtheriae. The patient recovered without incident after two weeks of treatment with diphtheria serum and penicillin.
This case further elucidates this underreported presentation of wound diphtheria mimicking a sexually transmitted genital ulcerative disease, and the authors emphasize the importance of considering diphtheria as distinct especially in atypical, long-term genital ulcers.
In 2013, the national diphtheria laboratory, Oberschleissheim and the Bavarian Health and Food Safety Authority, Oberschleissheim, Germany each reported a case of sexually transmitted diphtheria in a patient. non-gonococcal urethritis after genital exposure.
In October 2016, an adolescent boy suffered from acute genital ulcers in Cologne, Germany. The team believes it is a sexually transmitted disease, but initial diagnostic tests were negative.
The patient was hospitalized because the wound specimen grew Corynebacteria diphtheriae toxin, leading to the diagnosis of sexually transmitted diphtheria.

Measures to prevent diphtheria
Preventive measures
- Health education propaganda: In the regular health education propaganda work, it is necessary to provide necessary information about diphtheria to the people, especially mothers and teachers, so that they can detect it. Early detection, isolation, disease prevention and collaboration with medical staff to fully vaccinate children against diphtheria.
- Hygiene to prevent disease:
+ Houses, kindergartens, and classrooms must be airy, clean, and have enough light.
+ In places with old diphtheria outbreaks, it is necessary to strengthen surveillance and detect cases of pseudomembranous pharyngitis. If possible, swab the throat of former patients and people nearby to test for healthy carriers of the virus. diphtheria bacteria.
+ Organize full diphtheria vaccination according to the Expanded Program on Immunization. If possible, conduct a vaccination assessment once every 5 years and/or perform the Shick reaction to assess immunity status. diphtheria epidemic in the pediatric population.
Anti-epidemic measures
- Organization:
+ Establish an Anti-Epidemic Committee with government leaders as the head, local health leaders as the standing vice-committee and other relevant members such as: Health, Education, Police, Women's Union , Red Cross Society etc../p>
+ Members of the Anti-Epidemic Committee are assigned tasks to direct and mobilize the community to perform well the anti-epidemic work.
+ For small outbreaks, it is necessary to reserve a number of beds in a separate area in the hospital infection department to isolate and treat patients. If there is a major epidemic, a field clinic can be established in the community.
- Expertise:
+ Diphtheria is a disease that must be declared.
+ All patients with pseudomembranous pharyngitis suspected of diphtheria must be hospitalized for strict respiratory isolation until the results of two bacterial tests are available (-). Each specimen is taken at separate intervals. 24 hours and no more than 24 hours after antibiotic treatment. If testing is not possible, the patient must be isolated after 14 days of antibiotic treatment.
+ Management of healthy carriers and contacts: People who have close contact with the patient must be tested for bacteria and monitored within 7 days. Give a single dose of injectable Penicillin or oral Erythromycin every 7 to 10 days to people who have been exposed to diphtheria, regardless of their immune status. If the bacteria test is (+), they must be treated with antibiotics and take a leave of absence from work at schools or food processing facilities until the bacteria test results are (-).
+ Contacts who have been previously immunized should receive a booster dose of diphtheria toxoid.
+ Environmental treatment: Must disinfect and disinfect at the same time and final disinfection of all objects related to the patient. Disinfect and disinfect patient rooms daily with cresyl and chloramin B; Dishes, chopsticks, blankets, clothes... must be boiled; Books, notebooks, toys, etc. must be exposed to the sun.
Diphtheria prevention
To proactively prevent diphtheria, the Expanded Program on Immunization recommends that people well implement the following measures:
Take your child to be vaccinated, get a combination vaccine with complete diphtheria prevention ingredients, on schedule, including vaccinations when the child is under 1 year old and a booster vaccination when the child is 18 months old.
In high-risk areas, 7-year-old children need a 5th dose of reduced-dose diphtheria-tetanus (Td) vaccine.
In addition, it is necessary to maintain personal hygiene (regularly wash hands with soap; cover mouth when coughing or sneezing; clean nose and throat daily); Make sure houses, kindergartens, and classrooms are airy, clean, and have enough light.
People in the outbreak need to strictly comply with taking preventive medicine and getting vaccinated against diseases as prescribed and requested by health authorities.
Diphtheria vaccine vaccination schedule in the Expanded Immunization Program:
1st shot: Vaccinate DPT - HBV - Hib (to prevent diphtheria - pertussis - tetanus - hepatitis B - pneumonia/meningitis caused by Hib) when the child is 2 months old.
Shot 2: Vaccinate DPT - HBV - Hib when the child is 3 months old.
Shot 3: Vaccinate DPT - HBV - Hib when the child is 4 months old.
Shot 4: Vaccinate DPT (diphtheria - pertussis - tetanus) vaccine when the child is 18 months old.
How to treat laryngeal diphtheria?
Patients need to be actively treated at a medical facility. Delay in treatment of diphtheria can lead to many dangerous cardiovascular, neurological, kidney complications, airway obstruction leading to coma and death.
Toxigenic strains of C. diphtheria produce exotoxins that can cause damage to the mucosa of the respiratory tract, the skin (cutaneous diphtheria), and occasionally the mucosa of other sites (conjunctiva, ears, vulva). , vagina)…
Toxins destroy local tissue, form membranes and can be absorbed into the blood and distributed throughout the body leading to severe complications (such as myocarditis, neuritis, thrombocytopenia, kidney failure). Most occur in unvaccinated people.
Therefore, treatment of laryngeal diphtheria includes the use of diphtheria antitoxin and antibiotics.
Antibiotics are used to eliminate bacteria from infectious foci, preventing the diffusion and secretion of toxins.
However, antibiotics have no value in neutralizing diphtheria toxin and cannot replace antitoxin in treating the disease.
In cases where there are signs of airway obstruction, the doctor will prescribe pseudomembrane removal to clear the airway.
Intubation or tracheostomy may be needed and admission to the intensive care unit (ICU) for care may be required.
Supportive care includes: Cardiac monitoring – increased heart rate can cause cardiac arrest; infusion; bed rest; Management of systemic complications.

Drugs to treat laryngeal diphtheria
Diphtheria antitoxin
The earliest use of diphtheria antitoxin is the most important factor in the treatment of diphtheria, especially laryngeal diphtheria.
Because antitoxins do not neutralize toxins that have adhered to tissues, delaying their administration is associated with an increased risk of death. Therefore, it should be done as soon as possible to avoid complications.
The drug is used intravenously or intramuscularly. Hypersensitivity reactions including anaphylactic reactions, acute fever, and serum sickness may occur.
Therefore, extreme caution should be exercised when administering diphtheria antitoxin to people with a history of allergy and/or previous hypersensitivity. It is necessary to prepare adrenaline and other supportive measures to immediately treat an anaphylactic reaction if it occurs.
Antibiotics
Antibiotic treatment is often effective before the bacteria begin to release toxins into the bloodstream. It brings benefits such as: Reduces the amount of toxins released in the blood; Prevent the spread of infection.
Antibiotics commonly used in diphtheria infections are erythromycin and penicillin. Linezolid and vancomycin are also used in cases of antibiotic resistance.
Patients should adhere to a full course of antibiotics as advised by their doctor to completely eliminate the bacteria.
Other medications
Other medications such as corticosteroids, antihistamines, or adrenaline to reduce any severe reaction to the antitoxin are used.

Pay attention to the patient
- Eat a soft diet: Laryngeal diphtheria causes sore throat and difficulty swallowing. It is better to consume soft and liquid foods.
- Isolation: Because the disease is very contagious, it is necessary to isolate the patient to reduce the spread of the disease.
- Maintain hygiene: Those taking care of patients must maintain strict hygiene. Precautions such as hand washing should be followed, especially before cooking food and providing patient care.
- Vaccination: Vaccination is also necessary for patients who have recovered from diphtheria because the disease can occur again. Caregivers and people in close contact with the patient should also get a booster dose of the vaccine.
- Get enough rest: The patient's recovery is generally slow, especially if the infection is severe, so you should rest appropriately. Exertion can be harmful if the disease has already affected the heart.









 Facebook
Facebook
 Tweet
Tweet
 Zalo
Zalo







 News
News

















 Sign in with Facebook
Sign in with Facebook
 Sign in with Google
Sign in with Google